Opioids and Other Substances
Opioids and Other Substances
Middlesex-London’s Community Drug and Alcohol Strategy (CDAS) assists in preventing and addressing substance use-related harms in the community, such as opioids, which have had a significant impact in our community. Opioid deaths in Middlesex-London were stable through 2016 and 2017 while rates increased significantly in the province. However, preliminary data from 2018 shows an increase in the death rate from 2017. The 45–64 age group had the highest rates of death, which was different than emergency department visits where the 25–44 age group bore the highest burden. Males were significantly more likely to experience opioid-related emergency department visits and death, as were urban populations. Crack or cocaine was the most commonly used illicit drug closely followed by PCP, LSD or hallucinogens.
| Opioid-related Deaths | Use of Other Substances |
| Opioid-related Emergency Department Visits |
Opioid-related Deaths
Opioid-related death rates have fluctuated in Middlesex-London since 2005. In Ontario, the death rate slowly increased until 2017, when it jumped significantly (Figure 5.4.1). Middlesex-London did not see the same increase in 2017 as was seen in Ontario for opioid-related death rates. ML reported 31 deaths, similar to 2016. However, preliminary estimates for 2018 indicate higher death rates than in the past (not shown).
Although the differences between age groups were not significant, those in the 45–64 age group had the highest rate of death, followed by those in the 25–44 age group (Figure 5.4.2).
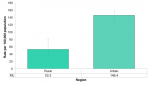
Males had three times the rate of deaths from opioid poisonings (9.0 per 100,000) compared to females (3.1) in Middlesex-London in the years 2015 to 2017. The difference was not statistically significant, likely due to small counts (Figure 5.4.3).
Interpretation
In a review of opioid-involved overdose deaths in the United States between 2013 and 2017 similar demographic factors for those most affected were observed compared to Middlesex-London.1 Males had a rate of opioid-related death, more than double females and there were no substantial differences between urban and rural populations. Higher death rates were observed in the 25–44 age group compared to the 45–64 group, which differs from the ML numbers. However small numbers in ML and non-significant differences may mean that the pattern observed is not actual.
Opioid-related Emergency Department Visits
The rate of emergency department visits related to opioids increased significantly between 2014 (79.8 per 100,000) and 2017 (146.8 per 100,000) after declining between 2010 and 2014. A similar pattern was seen in Ontario (Figure 5.4.4).
Males had nearly a 50% higher rate of opioid-related visits to the emergency department compared to females in 2017. The rate in males was 174.8 per 100,000 compared to 119.6 in females (Figure 5.4.5).
Those living in urban populations (146.4 per 100,000) had more than two and half times the rate of opioid-related emergency department visits compared to those in rural populations (53.3) (Figure 5.4.6).
Those in the 25–44 age group had significantly higher rates of ED visits for opioids (312.8 per 100,000) than any other age group. The rate for this age group was more than twice both the 15–24 age group (152.9) and the 45–64 age group (116.8). This pattern is different than what is observed in opioid-related deaths, where the 45–64 age group has the highest mortality, followed by the 25–44 group (Figure 5.4.7 and Figure 5.4.2).
Interpretation
The Middlesex-London Community Drug and Alcohol Strategy points out that from a health equity perspective, some populations are at higher risk for problematic substance use and substance use harms. These include Indigenous persons, people in correctional facilities, lesbian, gay, bisexual, transgender, queer or questioning (LGBTQ2+) youth, and those who are homeless or unstably housed.2
In young people, a study showed that those growing up in a lower social class, having received psychiatric care in hospital, witnessing family members overdose and past injection drug use were all predictors of a non-fatal opioid overdose.3
Use of Other Substances
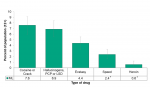
Crack or cocaine (7.6%) was the most commonly reported illicit drug that had been used by Middlesex-London residents in their lifetime. This was closely followed by hallucinogens such as PCP or LSD (6.9%). Ecstasy, speed and heroin were all reported by less than five percent of the population. Note that this data does not include opioids beyond heroin (Figure 5.4.8).
Population Health Assessment and Surveillance Protocol, 2018
References:
1. Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths - United States, 2013-2017. MMWR Morb Mortal Wkly Rep [Internet]. 2019 Jan 4 [cited 2019 Mar 26];67(51/52):1419–27. Available from: https://www.cdc.gov/mmwr/volumes/67/wr/mm675152e1.htm
2. Middlesex-London Community Drug and Alcohol Strategy Steering Committee. Middlesex-London community drug & alcohol strategy: a foundation for action [Internet]. London (ON): Middlesex-London Community Drug and Alcohol Strategy Steering Committee; 2018 Sept [cited 2019 Mar 26]. 60 p. Available from: https://static1.squarespace.com/static/599320d3b8a79baf4289fc66/t/5bc600...
3. Silva K, Schrager SM, Kecojevic A, Lankenau SE. Factors associated with history of non-fatal overdose among young nonmedical users of prescription drugs. Drug Alcohol Depend [Internet]. 2013 Feb 1 [cited 2019 Mar 26];128(0):104–10.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4184803/pdf/nihms630567.pdf Author’s manuscript.
Last modified on: May 7, 2019
Jargon Explained
Opioid-related death:
“acute intoxication/toxicity death resulting from the direct effects of the administration of exogenous substance(s) where one or more of the substances is an opioid, regardless of how the opioid was obtained.” Office of the Chief Coroner of Ontario
Opioid-related visit to ED:
All visits to the emergency department related to the opioids for either a poisoning by an opioid drug or a mental and behavioural disorder due to use of opioids. Some examples include acute intoxication, dependence syndrome, withdrawal state and psychotic disorder.