Cannabis
Cannabis
Cannabis is one of the most commonly used psychoactive substances in the province. Under the Ontario Public Health Standards, Public Health is mandated to prevent or delay cannabis use, and to reduce the harms associated with cannabis use. Prior to cannabis legalization, about half of the population reported lifetime use, even if only once, in Middlesex-London in 2015/16. At that time about one in six reported use in the past year. The most frequent users, those who used daily or a few times per week, made up about 6% of the population. Those aged 20 to 44 had the highest rate of reported lifetime use. Rates of cannabis-related visits to the emergency department have greatly increased since the early 2000s; there was more than a six-fold increase between 2004 and 2017. Males and those in the 15–24 age group had the highest rates.
| Cannabis Use | Cannabis-Related Emergency Department Visits |
Cannabis Use
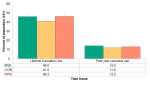
Nearly half (46.0%) of the Middlesex-London population aged 19 and older reported that they had used cannabis in their lifetime (including one time use) and 14% reported use in the previous 12 months in 2015/16. These rates are not statistically different from the province or the peer group (Figure 5.3.1).
Frequency of use indicates that about 6% of the Middlesex-London adult population (19 years and older) used daily or a few times a week in 2015/16. About 4% of adults reported using weekly or a few times a month and 4% used once a month or less (not shown).
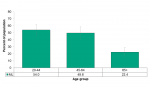
Those in the 20–44 age group reported a lifetime use of 54.0%, which was slightly higher than the 45–64 age group (49.6%). Both groups were significantly higher than those aged 65 and older reporting lifetime use (22.4%) (Figure 5.3.2).
Interpretation
Public Health is responsible for implementing and enforcing The Smoke Free Ontario Act, 2017 (SFOA, 2017). The SFOA, 2017 prescribes where the smoking of tobacco and cannabis, and the vaping of any substance, are banned in Ontario. Specifically, it outlines that one cannot smoke or vape cannabis in any enclosed workplace or public place, as well as many other outdoor places that are designated as smoke and vapour-free.1 With the legalization of cannabis in October, 2018 and the increased availability of legal cannabis products, understanding the proportion of the population currently smoking and vaping cannabis and those who are exposed to second-hand smoke provides valuable information about those at risk from the harms of cannabis use in the context of this legislation. There are a number of regulations controlling cannabis production, sale, consumption and possession of cannabis for the purposes of protecting public health and safety and keeping cannabis away from youth.2
Similar to Middlesex-London, the Centre for Addiction and Mental Health reported increases in the rate of cannabis use to about 1 in 6 (15%) in Ontario in 2015.3 This was a significant increase from 9% in 1996.
Cannabis-Related Emergency Department Visits
The rate of emergency department visits related to cannabis use increased dramatically between 2004 and 2017. The rate in 2017 was 74.5 visits per 100,000 population, more than a six-fold increase from the rate in 2004 (11.0 visits per 100,000) (Figure 5.3.3).
Between 2015 and 2016 there was a statistically significant increase in the rate of emergency department visits seen in Middlesex London. Between 2013 and 2015, Middlesex-London rates were significantly lower than Ontario; however, local rates caught up to provincial rates in 2016 and 2017. Middlesex-London rates have been consistently lower than the peer health units (Figure 5.3.3).
Poisonings related to cannabis use represent a small fraction of the total cannabis-related emergency department visits (~20%) compared to mental and behavioural disorders (~80%). Of particular concern are those very young children who may be ingesting cannabis, particularly when in the form of edibles such as candies or baked goods. The number of poisonings in those under age 10 was extremely small (not shown).
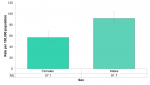
Males (91.7 per 100,000) had a statistically significantly higher rate of emergency department visits for cannabis use than females (57.1 per 100,000) in 2017 (Figure 5.3.4).
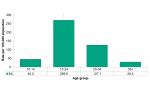
The 15–24 age group had, by far, the highest rate of cannabis-related emergency department visits (269.9 per 100,000) followed by the 25–34 age group (127.1 per 100,000). People aged 35 and older had very few emergency department visits related to cannabis poisoning or mental and behavioural disorders (Figure 5.3.5).
Interpretation
After cannabis was legalized in Colorado in 2014, trends showed the greatest proportion of people who visited the emergency department (95%) reported intentional use as opposed to unintentional. As well, those visiting the emergency department due to cannabis were more likely to have reported edible use rather than smoking cannabis. However, unintentional poisoning risk, particularly for children, may increase if the availability of the cannabis in households increases with legalization. Once edible cannabis products are legalized in 2019 this may become a larger concern. Emergency departments across the country are preparing to recognize signs and symptoms of cannabis poisoning in infants and children to assist in diagnosis.5
Other harms may result from cannabis use such as impaired driving and dependence. Research indicates that driving after cannabis use in Ontario adults increased between 2010 and 2015 from 2% to 3%. The increase was statistically significant. Men and the 18–29 age group contributed to those increases.2 In Ontario in 2015, 8% of the population reported moderate or high risk of cannabis problems according to the ASSIST-CIS (4+). Among users of cannabis it was 45%.2 The ASSIST-CIS (4+) tool, developed by the World Health Organization, assesses the risk of developing health, social, financial, legal, relationship or other problems with an individual’s current pattern of use.6
Population Health Assessment and Surveillance Protocol, 2018
References:
1. Ministry of Health and Long-Term Care [Internet]. Toronto (ON): Government of Ontario, Ministry of Health and Long-Term Care; c2012-2019. Where you can’t smoke or vape in Ontario; 2018 Oct 24 [modified 2019 Feb 20; cited 2019 Mar 27]; [about 8 screens]. Available from: https://www.ontario.ca/page/where-you-cant-smoke-or-vape-ontario
2. Department of Justice [Internet]. Ottawa (ON): Government of Canada, Department of Justice; [modified 2019 Mar 26]. Cannabis legalization and regulation; 2018 Oct 17 [cited 2019 Mar 22]; [about 5 screens]. Available from: https://www.justice.gc.ca/eng/cj-jp/cannabis/
3. Ialomiteanu AR, Hamilton HA, Adlaf EM, Mann RE. CAMH monitor ereport 2015: substance use, mental health and well-being among Ontario adults, 1977-2015 [Internet]. Toronto (ON): Centre for Addiction and Mental Health; 2016 [cited 2019 Mar 26]. 299 p. (CAMH research document series; no. 45). Available from: https://www.camh.ca/-/media/files/pdfs---camh-monitor/camh-monitor-2015-...
4. Marx GE, Chen Y, Askenazi M, Albanese BA. Syndromic surveillance of emergency department visits for acute adverse effects of marijuana, Tri-County Health Department, Colorado, 2016-2017. Public Health Rep [Internet]. 2019 Mar [cited 2019 Mar 22];134(2):132–40. Available from: https://journals.sagepub.com/doi/abs/10.1177/0033354919826562?rfr_dat=cr...
5. Murray D, Olson J, Lopez AS. When the grass isn’t greener: a case series of young children with accidental marijuana ingestion. CJEM [Internet]. 2016 Nov [cited 2019 Mar 22];18(6):480–3. Available from: https://www.cambridge.org/core/journals/canadian-journal-of-emergency-me...
6. WHO ASSIST Working Group. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction [Internet]. 2002 Sep [cited 2019 Apr 01];97(9):1183-94. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1360-0443.2002.00185.x...
Last modified on: May 7, 2019
Jargon Explained
Cannabis-related ED visit
These include visits for poisonings as well as cannabis-related mental health and behavioural reasons: acute intoxication; dependence; withdrawal; and, cannabis-related psychotic disorder.