Healthy Sexuality
Healthy Sexuality
The Government of Canada has developed targets to reduce the health impact of sexually transmitted and blood-borne infections (STBBIs). These targets were recently published in the format of a framework to guide action towards reaching groups of individuals who are undiagnosed and at high-risk for infection due to behavioural factors.1 Behaviours, such as unprotected intercourse, mouth-to-genital contact, early sexual debut (before the age of 20), having multiple sex partners, having sex with a partner who injects or has ever injected drugs, and being involved in sex trade work, are all associated with higher rates of sexually transmitted and blood-borne infections (STBBIs).2 Rates of STBBIs in Middlesex-London have risen since 2005; with rates of chlamydia in particular, rising sustainably above what was seen provincially as of 2018. More information on STBBIs and rates in Middlesex-London is available here.
A larger percentage of residents in Middlesex-London reported having an early sexual debut (under the age of 20) in comparison to Ontario. This pattern was also seen amongst individuals who reported having two or more sexual partners. Middlesex-London residents also reported a lower percentage of condom use the last time they had intercourse relative to both Ontario and the Peer Group. Individuals with post-secondary education reported a higher percentage of condom use compared to those with secondary or less than secondary education. Overall, the population in Middlesex-London at high-risk for STBBIs used a condom the last time they had intercourse as often as high-risk individuals across Ontario.
| Age of sexual debut | Condom use last time among those at risk for STBBIs |
| Number of sexual partners | Youth sexual activity |
| Condom use last time |
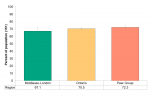
Age of sexual debut
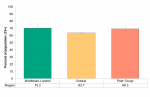
In 2015/16, Almost three-quarters (70.2%) of Middlesex-London residents reported having sexual intercourse for the first time before the age of 20 (Figure 6.7.1). This is significantly higher than the percentage in Ontario but not in the Peer Group.
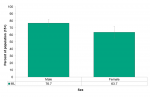
In general, males reported a higher percentage of sexual debut before the age of 20 compared to females in Middlesex-London (Figure 6.7.2).
The percentage of individuals having a sexual debut before the age of 20 was consistent across all the 5 quintiles of income in Middlesex-London (not shown).
No significant changes across the levels of household income seems to suggest no association between the income and having had an early sexual debut.
Interpretation
One of the behaviours associated with an increase in risk for STBBIs is starting sexual activity at a young age; the younger people are when they start having sex, the greater their risk is of getting STBBIs.3 This is noteworthy as STBBI rates for infections like chlamydia (Figure 9.1.4) and hepatitis C (Figure 9.1.10) are high in Middlesex-London in comparison to Ontario and young age is often associated with increased infection.3
Number of sexual partners
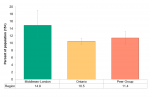
In 2015/16, approximately 15.0% of residents in Middlesex-London reported having more than one sexual partner in the past 12 months. This was significantly higher compared to both Ontario (10.5%) and the Peer Group (11.4%) (Figure 6.7.3). Both females and males in Middlesex-London reported similar percentages of having two or more partners, where females had lower percentages in Ontario and the Peer Group.
Approximately 71% of individuals living in urban locations in Middlesex-London reported having only one sexual partner in the past 12 months, which is significantly lower in comparison to those in rural parts of the region (81.0%) (not shown).
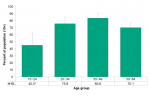
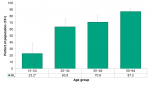
Youth and young adults between the ages of 15 and 24 often reported having more than one sexual partner in the last 12 months compared to other age groups. In fact, the percentage of having only 1 sexual partner in the past 12 months was higher in every bracket following this age group (25−34, 35−49, and 50−64) (Figure 6.7.4).
In addition to being over the age of 24, an increase in education (52.6% for no secondary education compared to 78.9% for post-secondary education) aligned with a higher percentage of Middlesex-London residents having only one sexual partner in the past 12 months (Figure 6.7.5).
Interpretation
Having multiple sex partners is associated with higher rates of sexually transmitted and blood-borne infections (STBBIs).4 Therefore, aside from using condoms, limiting the number of sexual partners is one of the other ways to avoid getting a sexually transmitted infection.5
As with an early sexual debut, the higher percentage of residents reporting more than 2 sexual partners in the past 12 months compared to Ontario raises questions about the risky sexual behaviours in Middlesex-London facilitating an increase in STBBI rates for infections like chlamydia (Figure 9.1.4) and hepatitis C (Figure 9.1.10). Middlesex-London has had higher rates of these infections compared to Ontario since 2005 and the gap has increased even more as of 2018.
Condom use last time
Approximately 67.1% of residents in Middlesex-London report having used a condom the last time they had sex in 2015/16 (Figure 6.7.6). This is slightly lower than the percentage in Ontario (70.5%) and Peer Group (72.3%). However, these differences are not statistically significant.
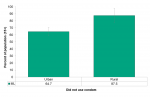
Residents in rural locations reported a significantly higher percentage of not using a condom the last time they had sex (87.5%) in comparison to individuals living in the urban locations (Figure 6.7.7).
In 2015/16, Middlesex-London residents age 15−24 reported the highest rates of using a condom the last time they had sex (76.7%) (Figure 6.7.8). However, they also reported the lowest percentage of having only 1 sexual partner in the last 12 months (Figure 6.7.4).
Those between the ages of 50 and 64 reported the lowest rates of condom use (12.8%) compared to younger individuals in Middlesex-London (not shown). However, this age group also report the highest percentage of no partners in the past 12 months (26.9%). These differences were not significantly significant.
Interpretation
Whether or not individuals use a condom greatly impact their risk of contracting a STBBI.6-8 Lower rates of condom use are often associated with a higher number of partners as well as an earlier sexual debut.5 This is illustrated in Middlesex-London, as seen in Figure 6.7.1 and Figure 6.7.3.
The lower rate of condom usage the last time among those aged 50−64 can be attributed to higher use of contraceptives, monogamous relationships or having no partners at all. In turn, this may have a close relationship to the low percentages of STBBIs among those ages 50−64 compared to the younger residents in Middlesex-London (Figure 9.1.3, Figure 9.1.5, Figure 9.1.9, Figure 9.1.12).
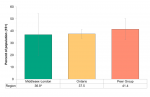
Condom use last time among those at risk for STBBIs
In 2015/16, condom use among those at high-risk for STBBIs in Middlesex-London was comparable to percentages in Ontario and the Peer Group (Figure 6.7.9). About 36.9% of residents in Middlesex-London who reported having more than 2 partners in the last 12 months reported using a condom the last time they had sex. Ontario and Peer Group residents reported using a condom the last time 37.5% and 41.4% of the time, respectively.
Interpretation
Lower rates of condom use are often associated with a higher number of partners as well as an earlier sexual debut.5 In addition, being high-risk or having a high-risk partner (multiple sex partners in the past 12 months) is also associated with higher rates of sexually transmitted and blood-borne infections (STBBIs).8 This highlights the importance of condom use particularly for individuals with multiple partners.
As with condom use among all residents in Middlesex-London, the slightly lower percentage of condom use among those at high-risk may facilitate an increase in STBBI rates in the region.
Youth sexual activity
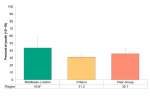
In 2015/16, youth (age 15−19) in Middlesex-London reported a higher percentage of sexual activity (43.6%) compared to Ontario (31.2%) and the Peer Group (35.7%) (Figure 6.7.10). However, this difference was not significantly different.
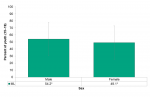
Male youth reported slightly higher percentages of having had sex (44.1%) than females (42.9%). Provincially, this difference was a little larger with 33.8% of male youth reporting having had sex compared to 28.3% of females (Figure 6.7.11).
Interpretation
These findings are consistent with Figure 6.7.1, which showed a higher percentage of the overall population in Middlesex-London reporting an early sexual debut as well as Figure 6.7.4, which showed that youth reported only having one sexual partner less often than older age groups. This highlights the relationship between starting sexual activity at a young age, an increased number of sexual partners, and the risk for genital herpes and other STIs.5
Population Health Assessment and Surveillance Protocol, 2018<
References
1. Government of Canada. Accelerating our response: Government of Canada five-year action plan on sexually transmitted and blood-borne infections [Internet]. 2019 Jul 17 [cited 2019 Oct 18]. Available from: https://www.canada.ca/en/public-health/services/reports-publications/acc...
2. HealthLinkBC. High-risk sexual behaviour [Internet]. 2018 [cited 2019 Sep 26]. Available from: https://www.healthlinkbc.ca/health-topics/tw9064
3. Upchurch DM, Mason WM, Kusunoki Y, Kriechbaum MJ. Social and behavioral determinants of self-reported STD among adolescents. Perspect Sex Reprod Health. 2004;36:276–87.
4. Unity Sexual Health. High risk groups [Internet]. 2017 [cited 2019 Sept 26]. Available from: https://www.unitysexualhealth.co.uk/our-services/high-risk-groups/
5. U.S. Food & Drug Administration. Condoms and sexually transmitted diseases [Internet]. 2018 Aug 01 [cited 2019 Oct 21]. Available from: https://www.fda.gov/patients/hiv-prevention/condoms-and-sexually-transmi...
6. Gallo MF, Steiner MJ, Warner L, Hylton-Kong T, Figueroa JP, Hobbs MM, et al. Self-reported condom use is associated with reduced risk of chlamydia, gonorrhea, and trichomoniasis. Sex Transm Dis. 2007;34:829–33.
7. Rietmeijer CA, Krebs JW, Feorino PM, Judson FN. Condoms as physical and chemical barriers against human immunodeficiency virus. JAMA. 1988;259:1851–3.
8. Smith DK, Herbst JH, Zhang X, Rose CE. Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2015;68:337–44.
9. Association of Public Health Epidemiologists in Ontario. Core indicators: Condom use the last time among those at risk for STDs [Internet]. 2004 Apr 27 [cited 2019 Sep 26]. Available from: http://core.apheo.ca/index.php?pid=134
Last modified on: November 19, 2019
Jargon Explained
Early sexual debut
Early sexual debut is defined as having sexual intercourse under the age of 20 the first time.9
“Condom use”
Individuals who reported that they used a condom the last time they had sex.9
“At risk for STBBIs”
Individuals who have had over two partners in the last 12 months and those whose relationships lasted less than 12 months.4,9