Preventable Mortality
Preventable Mortality
Preventable deaths are those deaths that could have been avoided by effective public health interventions along with a focus on the wider determinants of health, such as socioeconomic conditions and environmental factors. The reduction of avoidable deaths, including deaths considered preventable or treatable, is an important population health goal and a key indicator in measuring health system effectiveness.1,2,3,4
There were 600 deaths from preventable causes each year on average for Middlesex-London residents from 2013 to 2015. Preventable mortality improved significantly in Ontario from 2006 to 2015 and there was a similar trend in Middlesex-London. However, Middlesex-London’s preventable mortality rate was significantly higher than Ontario’s rate in 2015, after differences in age structure are taken into consideration.
There were significant subgroup variations in the rate of preventable mortality in Middlesex-London: higher for males than females and higher in the most materially deprived neighbourhoods compared with those in more well-off neighbourhoods.
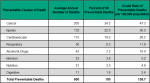
Over 75% of preventable deaths are attributable to cancer, injury and cardiovascular disease. Causes varied widely by age group; injury was common in the young, whereas chronic diseases such as cancer and cardiovascular disease were more common in the older age groups.
| Time trends in Preventable Mortality | Disease-specific preventable deaths |
| Preventable Mortality in Subgroups |
Time trends in Preventable Mortality
There were an estimated 600 deaths from preventable causes each year from 2013 to 2015 among residents of Middlesex-London.
Potentially preventable deaths in Middlesex-London fluctuated over the decade from 2006 to 2015, with a non-significant decrease overall in the ten-year period from 149.4 deaths per 100,000 to 135.3 deaths per 100,000 after accounting for changes in the population size and age structure. Middlesex-London’s rate was lowest in 2011 (121.3 per 100,000), a significant decline from 2006 (Figure 3.5.1).
During this same decade, a significant decrease in preventable mortality occurred in Ontario. Similarly, there was a significant decrease in the Peer Group (Figure 3.5.1).
Middlesex-London’s preventable mortality rate was higher than Ontario’s rate in most years and significantly higher in 2015. In contrast, it was lower, and some years significantly lower, than the Peer Group (Figure 3.5.1).
Interpretation
While preventable mortality improved over the past decade in Middlesex-London and Ontario, there is still potential to prevent approximately 600 deaths per year in Middlesex-London through more and better public health interventions and by addressing health inequities.
Preventable Mortality in Subgroups
Females had a significantly lower preventable mortality rate (99.6/100,000 population) than males (173.8/100,000 population) in Middlesex-London in 2015. The rate in females has been about half of that of the rate of males for each of the years reported between 2006 and 2015 (Figure 3.5.2).
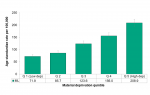
Preventable mortality increased with each material deprivation quintile and varied significantly by material deprivation quintile on average from 2011 to 2015. The rate for those that lived in the most well-off neighbourhoods was more than half (Q1 the least material deprived neighbourhoods; 71.9 per 100,000) that of the most materially deprived neighbourhoods (Q5 most material deprived neighbourhoods; 208.9 per 100,000). This is a rate difference of 137.0 deaths on average from 2011 to 2015 (Figure 3.5.3).
Interpretation
Preventable mortality varied significantly within both subgroups that were assessed. Mortality was higher in males and poorer neighbourhoods (i.e., most material deprived neighbourhoods). While efforts should be made to enable data collection and analysis by other subgroups at the health unit level, public health interventions could focus on improving preventable mortality in males and residents of poorer neighbourhoods.
Disease-specific preventable deaths
Cancer, injuries and cardiovascular diseases contributed to over three quarters of preventable deaths in residents of Middlesex-London from 2013 to 2015 (Figure 3.5.4).
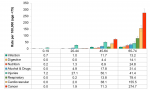
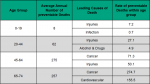
The specific preventable causes of death varied widely by age group in Middlesex-London from 2013 to 2015 (Figure 3.5.5).
Injuries were by far the most preventable cause of death for those aged 0-19, followed by infection from 2013 to 2015. For those aged 20-44, injury was also by far the most frequently reported preventable cause of death followed by alcohol and drugs. In those aged 45-64, injury slipped to second place behind cancer and in those 65-74, cancer and cardiovascular disease were the most frequently reported preventable cause of death (Figure 3.5.6).
Interpretation
Specific causes of preventable deaths can help to focus public health interventions. While the causes vary widely by age group, the greatest burden of preventable deaths were due to cancer, injuries and cardiovascular disease. Preventable causes of mortality may change over time with advances in population health interventions.
This preventable mortality indicator estimates the number of premature deaths from causes that could have been prevented (e.g., through changes in health behaviours or environmental supports); however, not all deaths that are classified as preventable could have actually been prevented.
Population Health Assessment and Surveillance Protocol, 2018
Ontario Public Health Standards: Requirements for Programs, Services, and, Accountability - Transparency and Demonstrating Impact (Figure 6, p.73)
References:
1. Government of Ontario, Ministry of Health and Long-Term Care. Ontario public health standards: requirements for programs, services, and accountability [Internet]. Toronto (ON): Ministry of Health and Long-Term Care; 2018 Jan 1 [revised 2018 Jul 1]. Figure 6, Public health indicator framework for program outcomes and contributions to population health outcomes; [cited 2019 May 27]; p. 73. Available from: http://www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/d...
2. Canadian Institute for Health Information; Statistics Canada. Health Indicators 2012 [Internet]. Ottawa (ON): Canadian Institute for Health Information; 2012 [cited 2019 Apr 7]. 128 p. Available from: https://secure.cihi.ca/free_products/health_indicators_2012_en.pdf
3. Allin S, Grignon M. Examining the role of amenable mortality as an indicator of health system effectiveness. Healthc Policy [Internet]. 2014 Feb [cited 2019 May 27];9(3):12-9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3999566/
4. Ministry of Health and Long-Term Care. Maintaining the gains, moving the yardstick: Ontario health status report, 2011 [Internet]. Toronto (ON): Queen’s Printer for Ontario; 2013 Feb [2019 May 27]. 58 p. Available from: http://www.ontla.on.ca/library/repository/ser/258918/2011.pdf
Last modified on: June 24, 2019
Jargon Explained
Preventable Mortality
refers to deaths from causes that can be potentially avoided by preventing a disease from developing. This includes deaths from conditions linked to modifiable risk factors, such smoking or excessive alcohol consumption (e.g., lung cancer, liver cirrhosis), and deaths linked to effective public health interventions (e.g., vaccinations, traffic safety legislation).