Self-harm & Suicide
Self-harm & Suicide
Suicide and self-harm are important issues with wide reaching effects in our communities. Rates of suicide have increased in recent years and emergency department visits for self-harm began climbing in 2012 after many years of reduction. About 10% of the population had seriously considered suicide in 2015 and 2016 while 2% reported making an attempt in their lifetime. Females and young people are more at risk for self-harm, however the pattern for suicide shows higher rates in males and those in their middle adult years.
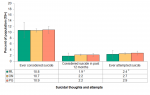
According to the Canadian Community Health Survey conducted in 2015 and 2016, one in 10 people, aged 15 and older in Middlesex-London, had seriously considered suicide at some time in their life (10.8%). The result is consistent with rates seen in the Peer Group and the province as a whole. Approximately 2% of the population had considered suicide in the year prior to the survey. Again, this rate was not different from the geographic comparators (Figure 4.6.1).
About 2% of the Middlesex-London population reported having attempted suicide in their lifetime (Figure 4.6.1).
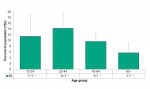
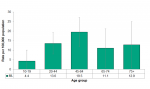
There were no significant differences seen by age group in those who had ever considered suicide. Although, the rates in those under age 44 were higher than those 45 and older (Figure 4.6.2).
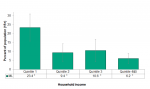
Those in the lowest income quintile had the highest rate of consideration of suicide in their lifetime (23.4%) in 2015/16, which was statistically significant from all other quintile groups. The trend shows that ever having considered suicide decreases as income increases with 6.2% of those in the top two quintiles reporting they had ever considered suicide (Figure 4.6.3).
There was no significant difference in suicide death rates between Middlesex-London and Ontario between 2008 and 2016 (Figure 4.6.4).
There appears to be an upward trend in rate of deaths from suicide in Middlesex-London between 2011 and 2016, although the change over time was not statistically significant. Small counts of suicide create large confidence intervals and therefore a substantial change in rates would be needed to see a statistically significant difference (Figure 4.6.4).
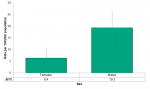
The rate of death due to suicide was three times higher in males (19.3 per 100,000) than in females (6.4). This difference was statistically significant (Figure 4.6.5).
The rate of deaths from suicide were highest in the 45-64 age group in Middlesex-London between 2014 and 2016, however the differences between age groups were not statistically significant due to the small numbers of events (Figure 4.6.6).
Rates of emergency department visits related to self-harm were declining between 2005 and 2011 but began to climb again between 2012 (161.1 per 100,000) and 2017 (223.9 per 100,000) (Figure 4.6.7).
The rate of ED visits for self-harm in 2017 were the highest of the time period between 2005 and 2017 and significantly higher than all other years except 2016 (Figure 4.6.7).
The upward trend in the past years was also mirrored in Ontario and the Peer Group but the rate at which Middlesex-London is increasing is greater than its comparators (Figure 4.6.7).
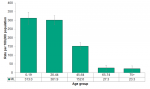
The youngest age groups had the highest rate of ED visits; 0-19 year olds (313.0 per 100,000) and 20-44 year olds (301.9). The trend decreases significantly with each age group until age 65 where the rate is less than 30 per 100,000 visits (Figure 4.6.8).
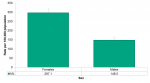
Females (297.1 per 100,000) had nearly double the rate of the emergency department visits for self-harm compared to males (148.5) in 2017 (Figure 4.6.9). No significant differences were seen between rural and urban populations (not shown).
The pattern of self harm visits to the emergency department by age group is much different than that observed for deaths by suicide. When comparing emergency department visits for self-harm to suicide deaths, females were more likely to go to the emergency department, whereas males were more likely to die (Figure 4.6.5 and Figure 4.6.9).
Interpretation:
Intentional injuries are those injuries that occur when someone brings harm to themselves or others. They account for 14% of the total costs associated with injuries in Ontario amounting to $1.2 billion in 2010. Suicide was the second largest cause of death due to injuries after falls. It’s impact was larger than transport collisions.1 It is important to note that self-harm and suicide attempts are not the same thing but self-harm may escalate to suicidal behavior.2
Seeing a health gradient by income quintile is common across different populations. Poverty in a large US cohort study was shown to be associated with suicide ideation, which was further amplified in the presence of mental illness.3 Sex differences have been demonstrated in studies about youth suicide ideation and attempts, with the risk in females being substantially and significantly higher than in males.4
Other studies have seen a rise in the rate of self-harm related emergency department visits between 2008 and 2015 in youth similar to trends seen in Middlesex-London. The increase was driven by females with rates in males showing no change between 2001 and 2015.5
Population Health Assessment and Surveillance Protocol, 2018
References:
1. Parachute. The cost of injury in Canada [Internet]. Version 2.2. Toronto (ON): Parachute; 2015 [2019 Feb 12]; 177 p. Available from: http://www.parachutecanada.org/downloads/research/Cost_of_Injury-2015.pdf
2. Canadian Mental Health Association, Centre for Suicide Prevention. A suicide prevention toolkit: self-harm and suicide [Internet]. Calgary (AB): Canadian Mental Health Association, Centre for Suicide Prevention; [2016 Oct?] [cited 2019 Feb 12]. 12 p. Available from: https://www.suicideinfo.ca/wp-content/uploads/2016/10/Self-Harm-Toolkit....
3. Pan YJ, Stewart R, Chang CK. Socioeconomic disadvantage, mental disorders and risk of 12-month suicide ideation and attempt in the National Comorbidity Survey Replication (NCS-R) in US. Soc Psychiatry Psychiatr Epidemiol [Internet]. 2013 Jan [cited 2019 Feb 12];48(1):71–9. Available from: https://link.springer.com/article/10.1007%2Fs00127-012-0591-9
4. Kokkevi A, Rotsika V, Arapaki A, Richardson C. Adolescents’ self-reported suicide attempts, self-harm thoughts and their correlates across 17 European countries. J Child Psychol Psychiatry [Internet]. 2012 Apr [cited 2019 Feb 12];53(4):381–9. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1469-7610.2011.02457
5. Mercado MC, Holland K, Leemis RW, Stone DM, Wang J. Trends in emergency department visits for nonfatal self-inflicted injuries among youth aged 10 to 24 years in the United States, 2001-2015. JAMA [Internet]. 2017 Nov 21 [cited 2019 Feb 12];318(19):1931–3. Available from: https://jamanetwork.com/journals/jama/fullarticle/2664031
Last modified on: March 15, 2019
Jargon Explained
Self-harm injuries
The group of injuries included in this category for emergency room visits are those where the individual purposely inflicted poisoning or injury on themselves. It also includes attempted suicide.
Income quintile
This is a measure that divides the entire population into five equal groups, also known as quintiles. Approximately 20% of the population is in each group. The lowest income quintile is the group with the lowest total household income, after taxes.
Small counts
The stability of a rate is dependent on the number of events that contribute to that rate. Therefore, rates in small populations are often unstable due to the relatively small number of events that occur each year. When comparing trends over time between Middlesex-London, the province and the Peer Group, we often see a larger fluctuation in rates locally than for Ontario, in which the trends are fairly smooth from year to year – this concept needs to be considered when interpreting the time trends and the confidence intervals in this resource.