Respiratory infections
Respiratory infections
Respiratory infections accounted for approximately 12% of all infectious diseases reported among Middlesex-London residents between 2005 and 2018. Influenza was the most common respiratory infection, with more than 4,000 cases reported across the 14-year time period. In contrast, the occurrence of other respiratory infections, such as legionellosis and active tuberculosis, was relatively low in Middlesex-London. As respiratory infections represent an important burden of illness, ongoing surveillance is required to monitor for emerging disease patterns, and as prevention, screening, diagnosis, and treatment practices evolve.
| Annual variation of respiratory infections | Active tuberculosis infections |
| Influenza | Other respiratory infections |
| Legionellosis |
Annual variation of respiratory infections
Between 2005 and 2018, influenza was by far the most common respiratory infection, with more than 4,000 cases reported among Middlesex-London residents across the 14-year time period. By comparison, the number of legionellosis and active tuberculosis cases was much lower, with fewer than 20 cases reported each year for each disease (Figure 9.2.1).
Influenza
View more information about influenza.
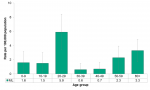
The rate of influenza infections was highest among seniors 60 years of age and over (275.8/100,000), followed by infants less than one year of age (209.4/100,000). The rates among these two age groups were significantly higher than rates in all other age groups (Figure 9.2.2).
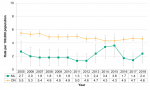
Rates of influenza infections increased significantly in Middlesex-London, from 20.6/100,000 in 2005 to 150.4/100,000 in 2018. The rate in Ontario also increased significantly over the same time period. From 2005 to 2010, the rate of influenza infections reported among Middlesex-London residents was lower than the Ontario rate. From 2011 to 2018, the local rate was significantly higher than the provincial rate in five of eight years, including the most recent three years (Figure 9.2.3).
Interpretation:
In the spring of 2009 a global influenza H1N1 pandemic emerged, with cases reported throughout the remainder of that year. At that time, cases were so numerous that from April 1, 2009 to January 31, 2010, provincial reporting requirements temporarily transitioned to aggregate reporting, rather than individual case reporting. As such, the rate of influenza cases reported in 2009 for both Middlesex-London and Ontario underrepresents the true incidence of influenza during that time because aggregate case counts are excluded.
Influenza is an infection characterized by changes in the strain that predominantly circulates each year. Seasons where influenza A(H3N2) circulates tend to have greater numbers of cases compared to those where influenza A(H1N1) or influenza B are more common. In addition, how well the seasonal influenza vaccine matches the strains of influenza that are circulating also impacts the number of cases that occur. Seasons where there is a good match between the influenza strains against which the vaccine protects and the circulating strains typically have lower numbers of cases.
Over the 14-year time period, the algorithms that health care providers have used to determine which patients to screen and test for seasonal influenza have been updated. Changes to these testing practices may influence the number of cases of influenza reported each year, as increased testing often leads to greater numbers of cases identified.
In addition to changes in screening and testing algorithms, laboratory methods for detecting influenza have also changed between 2005 and 2018. In 2009, Ontario public health laboratories began using a genetic testing method that was better able to detect influenza viruses compared to previous methods. This may have accounted for some of the increase observed in that year, and the general increasing trend in the rate of influenza cases from 2010 to 2018.
Legionellosis
View more information about legionellosis.
In Middlesex-London, rates of legionellosis infections was highest among those 60 years of age and over (3.2/100,000), followed by those 50-59 years of age (2.3/100,000) (data not shown).
Between 2005 and 2018, the rate of legionellosis infections increased among Middlesex-London residents, from no cases to 2.6/100,000, the highest rate in the 14-year time period. The rate for Ontario as a whole demonstrated similar increases. In most years the local and provincial rates were comparable; in four of 14 years the Middlesex-London rate was significantly lower than the Ontario rate (Figure 9.2.4).
Interpretation:
In 2009 the provincial case definition was updated to include new laboratory methods to test for legionellosis infections. This may have contributed to the peak in provincial rates in that year, as the new laboratory tests were less invasive, which may have increased the likelihood that symptomatic individuals would agree to be tested.
Active tuberculosis infections
View more information about active tuberculosis.
Among Middlesex-London residents, the rate of active tuberculosis infections was highest among those 20-29 years of age, at 5.9/100,000. The rate among those in their 20s was significantly higher than the rate among those under the age of 20 years, as well as those in their 30s and in their 40s (Figure 9.2.5).
Between 2005 and 2018, the rate of active tuberculosis cases in Middlesex-London fluctuated between 1.3/100,000 and 3.6/100,000. During the same time period, the Ontario rate generally declined, although the difference was not significant. Across the 14-year timeframe, the rate of active tuberculosis infections reported among Middlesex-London residents was consistently lower than the rate in Ontario; the difference was significant in all but two years (Figure 9.2.6).
Interpretation:
Between 2005 and 2018, the rate of active tuberculosis was low in Middlesex-London, and generally in Ontario as well. However, continued vigilance in screening and diagnosis of active tuberculosis is needed, since tuberculosis is prevalent in other parts of the world.1 Exposure to tuberculosis may be associated with travel to other countries, or resettlement of newcomers in Canada. As worldwide travel becomes more common, and as newcomers from other countries settle in Ontario, continued monitoring is important to ensure that rates do not begin to increase.
Other respiratory infections
View more information about blastomycosis and severe acute respiratory syndrome (SARS).
Between 2005 and 2018 there were no cases of blastomycosis or severe acute respiratory syndrome (SARS) reported among Middlesex-London residents (Figure 9.2.7).
Tuberculosis Prevention and Control Protocol, 2018
Population Health Assessment and Surveillance Protocol, 2018
References:
1. World Health Organization. Global tuberculosis report 2018 [Internet]. Geneva (Switzerland): World Health Organization; 2018 [cited 2019 May 30]. 277 p. Available from: https://www.who.int/tb/publications/global_report/en/ Licence: CC BY-NC-SA 3.0 IGO
Last modified on: July 25, 2019
Jargon Explained
Respiratory infections
Respiratory infections usually effect the lungs and other parts of the breathing system. Some respiratory diseases, like tuberculosis or blastomycosis, can cause infections in other parts of the body as well. Respiratory infections can be spread from an infected person to others through coughing, sneezing, or prolonged face-to-face interactions.