Other infectious diseases of public health significance
Other infectious diseases of public health significance
Many of the infectious diseases of public health significance are rare in Middlesex-London, such as acute flaccid paralysis, Creutzfeldt-Jakob disease, and hemorrhagic fevers. However, outbreaks of other diseases, including invasive group A streptococcus, have emerged in recent years. Ongoing efforts are needed to not only monitor for emerging clusters of rare infectious diseases, but to also inform public health action for infections that have increased in recent years and are affecting specific at-risk populations.
| Other infectious diseases of public health significance | Invasive group A streptococcus |
| Encephalitis and Meningitis |
Other infectious diseases of public health significance
View more information about acute flaccid paralysis (AFP), carbapenemase-producing Enterobacteriaceae (CPE), cholera, Creutzfeldt-Jakob disease (CJD), neonatal group B streptococcus, hemorrhagic fevers, leprosy, ophthalmia neonatorum, and smallpox.
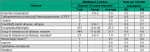
Between 2005 and 2018 there were no cases of carbapenemase-producing Enterobacteriaceae (CPE), cholera, leprosy, or smallpox reported among Middlesex-London residents. Cases of acute flaccid paralysis, Creutzfeldt-Jakob disease, hemorrhagic fevers, and ophthalmia neonatorum rarely occurred, with two or fewer cases reported for each across the entire time period. There were 27 neonatal group B streptococcus infections reported, corresponding to a rate of 37.1/100,000 among infants less than one year of age (Figure 9.7.1).
Interpretation:
Carbapenemase-producing Enterobacteriaceae infections have been reportable to public health only since May 2018, which accounts for the low numbers of this infection.
For neonatal group B streptococcus infections, the rate presented is for infants under the age of one year. This is because the provincial case definition applies only to newborns who are less than 29 days old.
Encephalitis and Meningitis
View more information about encephalitis / meningitis.
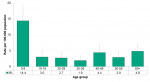
The rate of encephalitis/meningitis infections reported among Middlesex-London residents was highest among children under the age of 10 years, at 14.4/100,000. The rate in this age group was significantly higher than the rate in all other age groups (Figure 9.7.2).
Among Middlesex-London residents, the rate of encephalitis/meningitis cases decreased from 10.1/100,000 in 2005 to 4.1/100,000 in 2018. During the same time period, the rate for Ontario was relatively stable. The local rate generally exceeded the provincial rate, however, the Middlesex-London rate was comparable to the rate across Ontario from 2015 to 2018, the most recent four years (Figure 9.7.3).
Interpretation:
Rates of encephalitis/meningitis were highest among infants under 10 years of age. It is possible that this age group is more susceptible to the pathogens that cause encephalitis/meningitis, and truly experience a greater burden of illness. However, the elevated rate may be partially due to increased testing, and therefore more infections being detected. Health care providers may be more likely to test children who exhibit symptoms of encephalitis/meningitis than older individuals who have similar signs but may be better able to communicate, allowing them to help the health care provider narrow the possible diagnoses.
The rates of encephalitis/meningitis presented here underestimate the true occurrence of all encephalitis/meningitis cases. Most infectious diseases of public health significance are reported to public health based only on a positive laboratory result. Encephalitis/meningitis infections are reported based on the presence of signs and symptoms and a laboratory result that identifies a specific organism. Individuals who have symptoms of encephalitis/meningitis but whose illness is caused by an infectious disease of public health significance will be reported with the other disease. For example, a person experiencing encephalitis caused by West Nile virus would be reported as a West Nile virus case, not as an encephalitis/meningitis case.
Invasive group A streptococcus
View more information about invasive group A streptococcus.
The rate of invasive group A streptococcus infections was highest among those in their 30s and 40s (14.9/100,000 for both), followed closely by those in their 50s (14.8/100,000). The rates among these three age groups were significantly higher than rates among those under the age of 20 years (Figure 9.7.4).
From 2005 to 2015, the rate of invasive group A streptococcus infections in Middlesex-London was comparable to the Ontario rate. From 2016 to 2018, the local rate was significantly higher than the provincial rate, peaking in 2017 at 17.1/100,000 (Figure 9.7.5).
Interpretation:
In 2008 and 2012, clusters of invasive group A streptococcus infections were identified in Middlesex-London, largely among people who inject drugs (PWID). In 2016, a community outbreak of invasive group A streptococcus infections was declared in Middlesex-London, with cases continuing to be reported through 2017 and 2018. Nearly one-half of all cases were people who used drugs (PWUD) and/or were underhoused.1
Since 2016, PWUD and those who are underhoused have also been impacted by other infectious disease outbreaks, including HIV/AIDS, hepatitis A, and hepatitis C. In response, the Middlesex-London Health has worked collaboratively with health care providers and other community agencies to address these overlapping outbreaks among high risk groups.
Infectious Diseases Protocol, 2018
Population Health Assessment and Surveillance Protocol, 2018
References:
1. Dickson C, Pham MT, Nguyen V, Broacher C, Silverman MS, Khaled K, Hovhannisyan G. Community outbreak of invasive group A streptococcus infection in Ontario, Canada. Can Commun Dis Rep [Internet]. 2018 Jul 5 [cited 2019 May 31];44(7/8):182-8. https://doi.org/10.14745/ccdr.v44i78a06
Last modified on: July 26, 2019